By Renova Hospitals
January 17, 2026
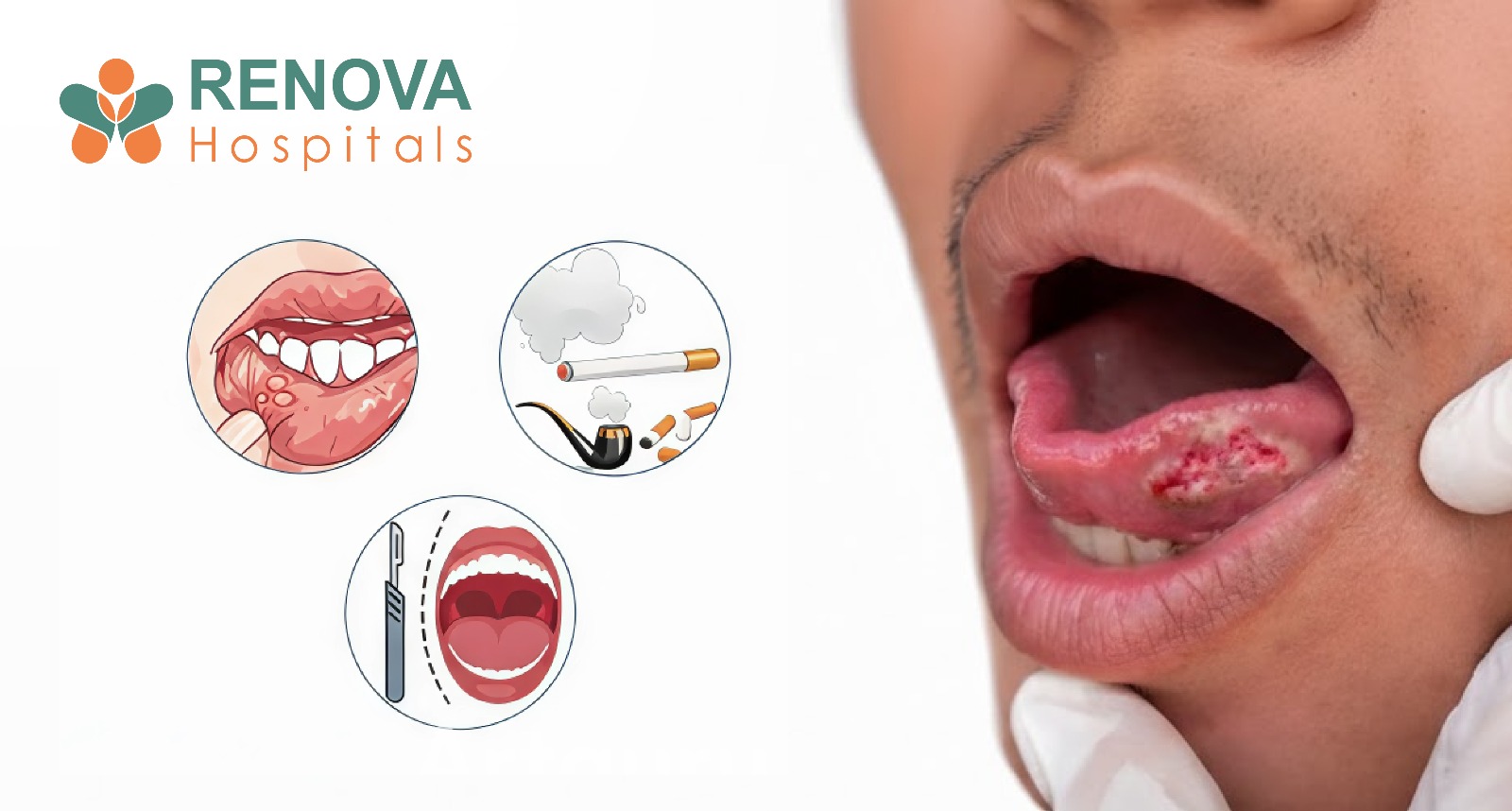
Ulcers Explained: Causes, Symptoms & Treatment of Mouth, Tongue and Stomach Ulcers
What Is the Role of the Digestive and Mucosal Lining?
- Pain or burning sensation
- Difficulty eating or swallowing
- Bleeding or soreness
- Increased sensitivity to spicy or acidic foods
What Are Ulcers?
- Oral ulcers (mouth, tongue, throat)
- Gastric and duodenal ulcers (stomach and intestine)
- The cause of tissue damage
- Depth of the ulcer
- Duration before treatment
- The person’s immune and nutritional status
Types of Ulcers
- Burning or tingling before the ulcer appears
- White or yellow centre with a red border
- Pain while eating or speaking
- Sharp pain on tongue movement
- Difficulty swallowing
- Referred ear pain
- Burning or gnawing abdominal pain
- Bloating or nausea
- Pain that worsens on an empty stomach
- Black stools or vomiting blood in severe cases
What Are the Symptoms of Ulcers?
- White/yellow sores with red borders on cheeks, lips, tongue, or gums.
- Sharp pain when eating, drinking, or speaking.
- Swelling, excess saliva, bad breath, and minor bleeding.
- Fever or swollen lymph nodes in severe cases.
- Dull, burning pain in the upper middle abdomen, worse after eating.
- Bloating, heartburn, nausea, vomiting, "coffee grounds".
- Appetite/weight loss, dark stools from bleeding.
- Burning pain 2-3 hours after meals or at night.
- Relieved temporarily by food/antacids.
- Bloating, belching, feeling overly full, and fatigue.
- Persistent or worsening pain
- Bleeding from the mouth or in the stools
- Unintentional weight loss
- Difficulty swallowing
- Vomiting blood or black stools.
What Causes Ulcers?
- Physical trauma or biting
- Accidental cheek or tongue biting, sharp teeth, ill-fitting dentures, or dental procedures can injure the lining and trigger ulcer formation.
- Stress and fatigue
- Prolonged stress and insufficient sleep weaken the immune response and impede tissue repair, increasing the risk of ulcer development or recurrence.
- Nutritional deficiencies
- Low levels of iron, vitamin B12, or folate impair cell regeneration and are a common cause of recurrent mouth and tongue ulcers.
- Bacterial infections (H. pylori)
- Helicobacter pylori damages the stomach’s protective lining and is a major cause of peptic and stomach ulcers.
- Long-term painkiller use
- Frequent use of NSAIDs such as aspirin or ibuprofen reduces protective mucus in the stomach, increasing ulcer risk.
- Smoking and alcohol
- Tobacco and alcohol irritate the mucosal lining, delay healing, and increase acid production.
- Acid overproduction
- Excess stomach acid can erode the gastric or duodenal mucosa, leading to ulcer formation.
Are Ulcers Contagious?
- Non-infectious ulcers
- Ulcers caused by stress, nutritional deficiencies, trauma, acid damage, or medications cannot spread through contact.
- Infection-related ulcers
- Ulcers caused by viral or bacterial infections may spread through:
- Close personal contact
- Sharing utensils, cups, or toothbrushes
- Poor hand hygiene
- Stomach ulcers and H. pylori
- While the ulcer itself is not contagious, the Helicobacter pylori bacterium that causes some stomach ulcers can be transmitted through contaminated food, water, or saliva.
- Good oral hygiene reduces risk.
- Regular handwashing, avoiding the sharing of personal items, and maintaining oral hygiene help reduce the spread of infection-related ulcers.
Diagnosing ulcers is essential to determine their type, cause, and severity and to rule out serious underlying conditions. Because ulcers can occur in different locations, such as the mouth, tongue, throat, or stomach, doctors tailor investigations based on symptoms, duration, and response to initial treatment.
- Location, size, and appearance of the ulcer
- Pain pattern (with eating, swallowing, or at rest)
- Duration and frequency of recurrence
- Associated symptoms such as weight loss, bleeding, or fever
- Iron, vitamin B12, and folate levels
- Infection or inflammation markers
- Autoimmune indicators
- Anaemia due to chronic blood loss
- Visualise stomach and duodenal ulcers
- Assess bleeding or scarring.
- Detect peptic ulcers
- Test for Helicobacter pylori
- Ulcers persist beyond 2–3 weeks.
- Irregular edges or unexplained bleeding are present.
- Malignancy must be ruled out.
- Breath test
- Stool antigen test
- Biopsy-based testing
- Detect perforation
- Assess the surrounding organs.
- Identify deep infections
- Oral infections
- Acid reflux disease
- Oral cancer
- Inflammatory bowel disease
- Fungal infections
Complications of Untreated Ulcers
- Chronic pain
- Ongoing irritation and inflammation can cause persistent discomfort, affecting eating, speaking, and daily activities.
- Secondary infection
- Open ulcers can become infected by bacteria or fungi, delaying healing and worsening symptoms.
- Bleeding
- Ulcers may erode blood vessels, leading to bleeding from the mouth or gastrointestinal tract, which can cause anaemia.
- Scarring
- Repeated or deep ulcers can heal with scar formation, potentially affecting tissue function.
- Stomach perforation
- In severe gastric or peptic ulcers, the ulcer can create a hole in the stomach wall, which is a medical emergency.
- Malnutrition
- Pain, poor appetite, and impaired digestion can reduce food intake and nutrient absorption over time.
Ulcer Treatment
- Topical medications and mouth ulcer gel
- Pain relief and anti-inflammatory medicines
- Nutritional supplementation
- Avoiding spicy and acidic foods
- Prescription medications
- Antibiotics if infection is present
- Acid suppression therapy
- Hospital care for bleeding ulcers
Self-Care Tips
- Control conditions, such as diabetes or stress that exacerbate ulcers.
- Take PPIs and antibiotics exactly as prescribed.
- Avoid caffeine, alcohol, tobacco, spicy foods, and NSAIDs.
- Maintain a healthy weight with small, bland meals (oatmeal, bananas, yoghurt).
- Eat last meal 3-4 hours before bed.
- Manage stress through yoga, walking, and meditation; sleep 7-8 hours.
- Severe, unrelenting abdominal pain.
- Vomiting blood/coffee grounds.
- Black tarry stools.
- Fainting, dizziness, and shortness of breath.
- Unexplained weight loss, persistent
How to Prevent Ulcers?
Prevent ulcers with these crisp, daily habits to protect your mouth and gut.
- Brush twice daily with a soft toothbrush; floss gently.
- Rinse with warm saltwater after meals.
- Choose yoghurt, bananas, oatmeal, and boiled veggies.
- Skip spicy, citrus, fried foods, chocolate, and fizzy drinks.
- Chew slowly; use a straw for lip sores.
- Quit tobacco; limit alcohol to 1 drink/day.
- Sleep 7-8 hours; de-stress with yoga/walks.
- Use NSAIDs sparingly with food; prefer paracetamol.
- Treat H. pylori infections promptly.
When Should You Seek Medical Care?
- An ulcer that does not heal within 2 weeks
- Frequent or recurring ulcers, especially in the same location
- Severe or increasing pain that interferes with eating or swallowing
- Bleeding from the mouth or blood in the stools
- Black stools or vomiting blood, which may indicate a stomach ulcer
- Difficulty swallowing or speaking
- Unexplained weight loss or fatigue
- Fever or signs of infection around the ulcer
- Ulcers occurring in children, elderly individuals, pregnant women, or people with weak immunity
Care at Renova Hospitals
Renova Hospitals offer comprehensive care for all ulcer types, ensuring personalised treatment from diagnosis to recovery. For oral ulcers, they provide targeted medications, such as soothing topical gels, alongside nutritional interventions to address deficiencies in vitamins B12, iron, or folate, thereby promoting faster healing and preventing recurrence.
In cases of persistent or complicated ulcers, the hospital implements close monitoring to prevent complications such as bleeding, perforation, or scarring and employs thorough infection control measures, including antibiotics, to ensure complete eradication. This integrated approach at Renova Hospitals minimises long-term complications and supports overall digestive health.
Category
- Joint Replacement
- Joint Replacement
- Joint Replacement