Overview
An
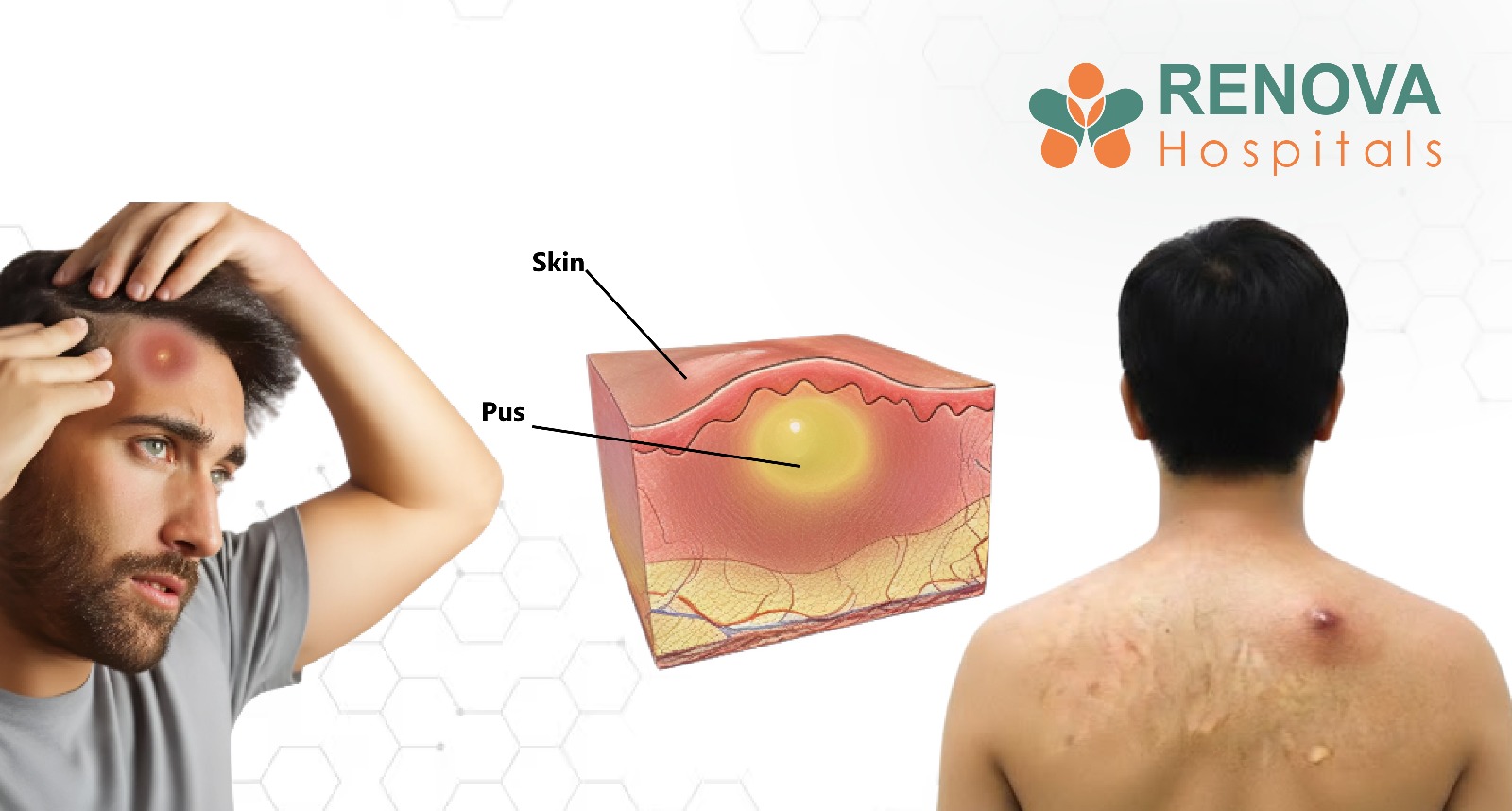
abscess is not just a painful lump or swelling; it is a sign that the body is fighting a bacterial infection. Many people are familiar with skin abscesses, which appear as visible, tender swellings filled with pus. These are often mistaken for pimples, boils, or insect bites and may be ignored or treated at home. While some skin abscesses resolve with basic care, others require medical treatment to prevent the infection from spreading.
What is less commonly understood is that abscesses can also develop inside the body. An internal abscess forms deep within tissues, organs, or body cavities and may not produce visible external signs. Because of this, internal abscesses are often diagnosed late and can lead to serious, sometimes life-threatening complications if not treated promptly.
This blog explains the key differences between skin abscesses and internal abscesses, covering symptoms, causes, diagnosis, and treatment in detail. Special attention is given to internal rectal abscess, a common but frequently delayed diagnosis. Understanding these differences helps patients recognise warning signs early and seek the proper medical care.
What Is an Abscess?
An abscess is a localised collection of pus that forms as a result of bacterial infection. When bacteria enter the body, the immune system responds by sending white blood cells to the infected area. These cells attack the bacteria, leading to tissue breakdown and the accumulation of pus, which consists of dead cells, bacteria, and inflammatory debris.
Abscesses can form almost anywhere in the body and are broadly classified into two main types:
- Skin abscess – occurs on or just below the surface of the skin
- Internal abscess – develops deep inside the body, often within organs or internal tissues
Although both types involve infection and pus formation, their presentation, severity, and treatment differ significantly.
Skin Abscess
What Is a Skin Abscess?
A skin abscess is a painful, pus-filled swelling that develops in or under the skin. It is usually well-defined, tender to the touch, and may gradually increase in size over days. Skin abscesses are among the most common soft-tissue infections seen in clinical practice.
Because skin abscesses are visible, they are often detected early. However, inappropriate home treatment, such as squeezing or puncturing, can worsen the infection and lead to complications.
What are the Symptoms?
Typical abscess symptoms in the skin include a combination of local and systemic signs:
- Red, swollen lump on the skin
- Pain and tenderness at the site
- Warmth over the affected area
- Tight, shiny, or stretched skin
- Visible pus or fluid drainage
- Throbbing or pulsating pain
- Fever and chills in severe cases
- Swollen lymph nodes near the infection
As the abscess matures, the centre may soften and appear yellow or white due to the accumulation of pus.
Internal Abscess
What Is an Internal Abscess?
An internal abscess is a pus-filled infection that develops deep within the body, often involving organs or internal spaces. Because it is not visible from the outside, symptoms are usually vague, leading to delayed diagnosis.
Internal abscesses can occur in various locations, including:
- Abdomen
- Pelvis
- Liver
- Lungs
- Brain
- Around the rectum and anus
Internal Abscess Symptoms
Internal abscess symptoms are usually less specific than skin abscess symptoms and may include:
- Persistent or unexplained fever
- Deep, localised pain
- Fatigue and weakness
- Loss of appetite
- Nausea or vomiting
- Night sweats
- Unexplained weight loss
- General feeling of illness
Because these symptoms mimic many other conditions, imaging tests are often required for diagnosis.
Internal Rectal Abscess
What Is an Internal Rectal Abscess?
An internal rectal abscess forms in the deep tissues around the anus or rectum. Unlike superficial perianal abscesses, internal rectal abscesses may not cause visible swelling, making diagnosis more challenging.
Internal Rectal Abscess Symptoms
Common internal rectal abscess symptoms include:
- Deep rectal or pelvic pain
- Pain during bowel movements
- Constant rectal pressure or fullness
- Fever and chills
- Difficulty sitting or walking
- Pain that worsens at night
- Sometimes, there is no external lump or redness
If untreated, an internal rectal abscess can lead to fistula formation, chronic infection, or sepsis.
What are the Causes of skin vs. internal abscesses?
Causes of Internal Abscess
Internal abscesses usually result from:
- Spread of infection from nearby organs
- Untreated skin or rectal infections
- Gastrointestinal conditions such as Crohn’s disease
- Appendicitis or bowel perforation
- Post-surgical infections
- Trauma to internal organs
- Bloodstream infections seeding internal tissues
What Happens Inside the Body
The formation of an abscess follows a predictable sequence:
- Bacteria invade tissues or organs
- Immune cells gather at the infection site
- Tissue breaks down, forming pus
- Pressure builds in confined spaces
- Surrounding tissues or organs become damaged
- Infection may spread into the bloodstream if untreated
This process explains why internal abscesses are often more dangerous than skin abscesses.
Causes of Skin Abscesses
Understanding the causes of skin abscesses helps prevent and treat them early. Common causes include:
- Bacterial infection, most commonly Staphylococcus aureus
- Blocked sweat glands or sebaceous glands
- Infected hair follicles or ingrown hairs
- Minor cuts, scratches, or insect bites
- Poor skin hygiene
- Excessive sweating and friction
- Diabetes mellitus
- Weakened immune system
- Repeated skin trauma or shaving
People with chronic illnesses or weakened immune systems are at higher risk of recurrent skin abscesses.
Diagnosis of Skin vs Internal Abscess?
Distinguishing between a superficial (skin) abscess and a deep (internal) abscess is vital, as one may be treated with a simple office procedure. In contrast, the other often requires hospitalisation and advanced imaging.
Diagnosis of Skin Abscess
Physical Examination
The clinician looks for the classic signs of inflammation: rubor (redness), calor (warmth), and tumour (swelling).
Inspection for Redness and Pus
If the skin is stretched thin and a yellowish or white centre is visible, it confirms that the infection has localised. This helps the provider decide if it is ready for incision and drainage (I&D).
Pus Culture and Sensitivity
For abscesses that keep coming back or don't respond to standard antibiotics, a sample of the pus is sent to a lab. This "culture" identifies specific bacteria (like MRSA) and determines which antibiotics will actually kill them, moving treatment from guesswork to precision.
Diagnosis of Internal Abscess
Blood Tests (Infection Markers)
Blood work usually shows an elevated White Blood Cell (WBC) count and high levels of C-Reactive Protein (CRP) or Erythrocyte Sedimentation Rate (ESR), which are general indicators of significant internal inflammation.
Ultrasound Evaluation
This is often the first line of defence for abdominal or pelvic concerns because it’s quick and radiation-free. It’s particularly effective for spotting fluid collections in the gallbladder, liver, or female reproductive organs by bouncing high-frequency sound waves off the internal structures.
CT Scan or MRI
provides a high-resolution, 3D map of the body, allowing doctors to see the exact size of the abscess and its proximity to major blood vessels or nerves.
Rectal or Pelvic Examination
In cases where an abscess is suspected near the bowel or reproductive tract (like a perianal or tubo-ovarian abscess), a manual internal exam is necessary.
Treatment of Skin Vs Internal Abscess?
Treatment of Skin Abscess at Home
If you catch a skin abscess in its very early "pimple-like" stage, you might be able to encourage the body to heal itself. However, this is only for minor, superficial bumps.
Warm Compresses
Applying a clean, warm washcloth to the area for 10–15 minutes several times a day is the most effective home remedy.
Hygiene and Protection
Keeping the area clean and dry prevents secondary infections from moving in. It’s best to cover the area with a loose, sterile bandage to protect it from friction against clothing—the golden rule: Never squeeze or pop it.
Monitoring for Red Flags
Home care is a "wait and see" game. You must watch for spreading redness (streaks), increased throbbing, or a fever. If the skin around the abscess becomes hard or the pain prevents you from sleeping,
Professional Treatment of Skin Abscesses
While small, early-stage bumps can sometimes be managed with warm compresses, most established skin abscesses require a clinical approach to prevent the infection from spreading into the bloodstream.
- Incision and Drainage (I&D)
- Wound Packing
- Oral Antibiotics
- Proper Wound Aftercare
Treatment of Internal Abscess
Because internal abscesses are confined within the body's cavities, they require a much more aggressive, sterile approach. There is no "home remedy" for an infection deep inside an organ.
Image-Guided Drainage
Using an ultrasound or CT scan as a real-time map, a radiologist inserts a thin needle or catheter through the skin and directly into the abscess to suction out the pus.
Surgical Drainage
A surgeon must manually clean the infected space and, if needed, place a temporary drain to prevent fluid from accumulating again.
Intravenous (IV) Antibiotics
Internal infections are more complicated for the body to wall off, so high-dose antibiotics are delivered directly into the bloodstream.
Hospitalisation and Monitoring
Recovery from an internal abscess usually happens in a hospital bed. Doctors need to constantly monitor your vitals, such as heart rate and temperature, to ensure you aren't developing sepsis.
Complications of Untreated Abscess
If not treated appropriately, both skin and internal abscesses can lead to:
- Spread of infection to surrounding tissues
- Bloodstream infection (sepsis)
- Chronic pain and scarring
- Fistula formation (especially rectal abscess)
- Organ damage
- Recurrent infections
When Should You See a Doctor?
Seek medical care immediately if:
- A skin abscess is increasing in size or causing pain
- Fever accompanies swelling
- Pus continues to drain
- Symptoms suggest an internal abscess
- Rectal pain is associated with fever
- Home treatment fails to improve symptoms
- Abscesses recur frequently
Prevention of Skin and Internal Abscess
Preventing an abscess, whether on the surface or deep inside, focuses on blocking the entry and supporting your body's natural defence systems.
- Maintain Personal Hygiene
Wash your hands frequently and bathe regularly to reduce the bacterial load on your skin, which lowers the risk of staph entering a pore or hair follicle. - Treat Skin Wounds Early
Clean even minor cuts or scrapes immediately with soap and water, and keep them covered; an open wound is an invitation for an abscess to form. - Avoid Squeezing Boils
Resist the urge to pop or squeeze any skin bump, as this can force the infection deeper into the tissue or even into your bloodstream. - Manage Diabetes Effectively
High blood sugar can weaken the immune system and slow healing; keeping glucose levels stable helps your body fight off localised infections before they turn into abscesses. - Complete Prescribed Antibiotics
Always finish a full course of antibiotics even if you feel better; stopping early can allow surviving bacteria to multiply and form a secondary, more resilient abscess. - Seek Care for Persistent Symptoms
Don't ignore localised pain, unexplained fever, or swelling; early medical intervention can stop an internal infection from "walling off" into a dangerous abscess.
Renova Hospitals: Expert Care for Skin and Internal Abscess
We specialise in providing straightforward answers and effective relief for patients dealing with everything from painful skin infections to complex internal abscesses. We understand that an abscess, especially a sensitive internal or rectal one, can be both physically taxing and stressful, which is why our approach combines advanced technology with a compassionate, human touch.
Our facility takes the guesswork out of deep-seated infections by utilising high-definition imaging, e.g., CT scans and MRIs, to pinpoint the exact location of internal issues. Whenever possible, we prioritise minimally invasive, image-guided drainage, which means smaller incisions, less discomfort, and a much faster return to your daily life.
From managing specialised rectal cases with the utmost privacy to providing targeted IV antibiotics and meticulous aftercare, our multidisciplinary team stays by your side until the infection is completely cleared and your health is fully restored.
Disclaimer
This content is for general information only and does not replace professional medical advice. Always consult a qualified doctor for diagnosis and treatment.