By Renova Hospitals
January 28, 2026
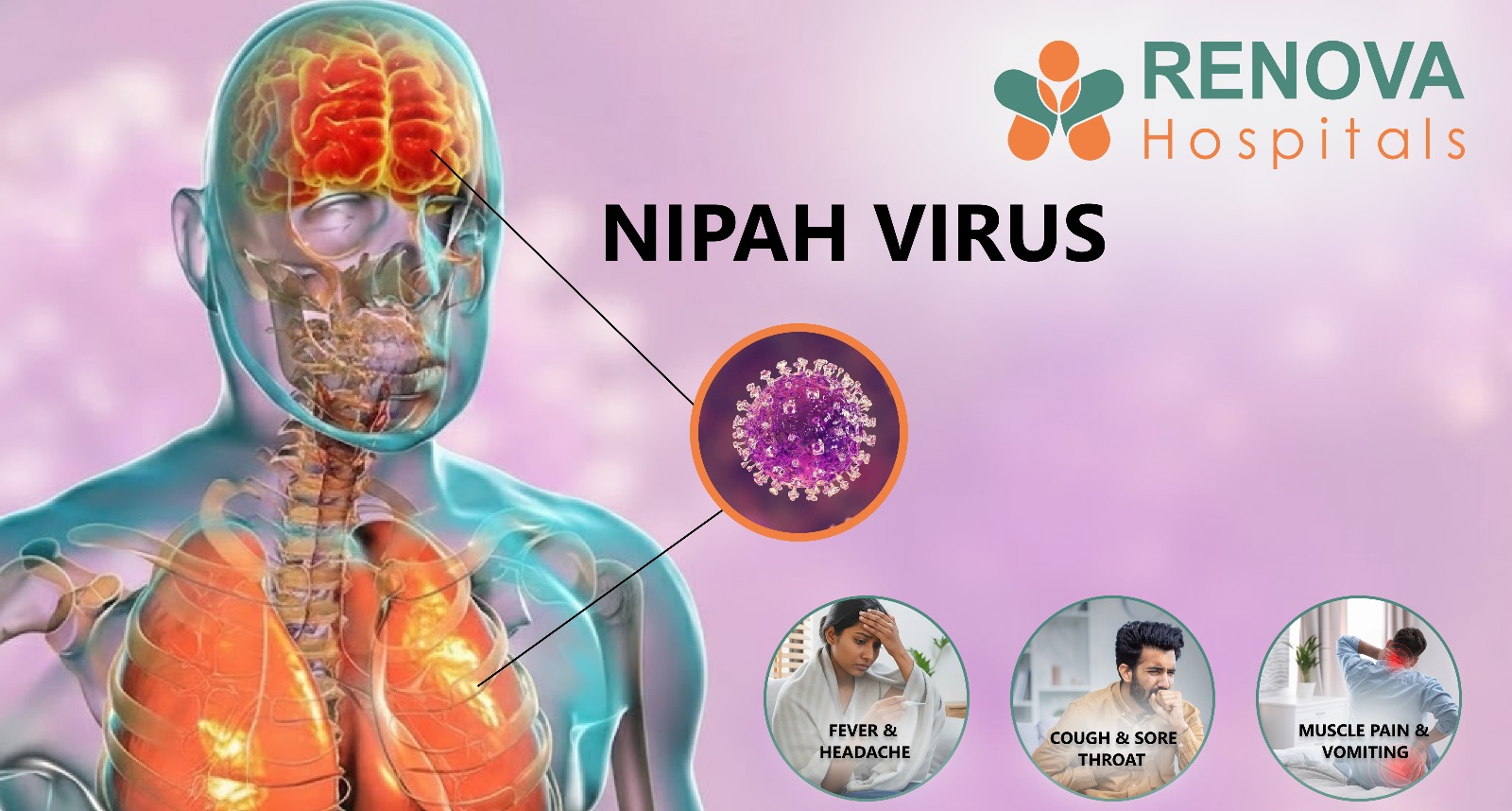
Nipah Virus : Symptoms, Causes, Transmission, Treatment & Prevention
Overview
People in India often call it an infectious disease, and it keeps coming back in groups, so early detection and strict prevention are essential.
What is the Nipah virus?
The first time the virus was found was during a Nipah virus outbreak in Malaysia in 1998. Since then, India has had several outbreaks, mainly in Kerala.
Where can you find the Nipah virus?
- The Natural Reservoir
- The fruit bat Pteropus, often called a "flying fox," is the primary host of the Nipah virus. It has a virus, but don't get sick. They spread the virus through their saliva, urine, and poop, which can make the environment or food sources unsafe.
- The Nipah virus doesn't live everywhere; it usually lives in certain "hotspots" and places:
- Geographic Hotspots: Bangladesh and India (especially Kerala) have many outbreaks. In the late 1990s, it was in Malaysia and many other places.
- Food contaminated with the virus: The virus is often found in raw date palm sap collected in contaminated collection containers. This leaves behind infected fluids that people then drink.
- Intermediate Hosts: The virus is found in bats, but it is also common in pigs on farms. During the first outbreak in Malaysia, the virus went from bats to pigs and then to people.
- Fruit orchards or farms where bats and people live close to each other are places where the virus is most likely to be found in proximity to the virus (NiV)
Characteristics of the Nipah virus?
- Zoonotic Character: It belongs to the Henipavirus genus and is naturally found in fruit bats (Pteropus genus). It can jump directly to humans or other animals, such as pigs.
- High Virulence: It is one of the most deadly viruses known, with a Case Fatality Rate (CFR) of 40% to 75%.
- Incubation Period: The virus's incubation period can be anywhere from 4 to 14 days, but it can also last up to 45 days. This "silent" phase makes it hard to keep things under control.
- Neurological Effects: One of the main signs of NiV is acute encephalitis, which can cause fever, headache, mental confusion, and, in the worst cases, seizures and coma.
- Respiratory Distress: Many patients have severe respiratory problems, such as acute respiratory distress syndrome (ARDS), which makes it easier for the virus to spread from person to person through droplets.
- Long-term sequelae: Survivors may experience enduring neurological disorders, including alterations in personality or "smouldering" encephalitis, which can recur months or even years post-recovery.
What Causes the Nipah Virus?
How does the Nipah virus spread?
- Touching bats or pigs that are sick
- Eating or drinking fruits or drinks that are tainted
- Transmission between humans through respiratory droplets and bodily fluids
- The "Spillover" Event: A "spillover" from fruit bats to people or animals is often the first step in transmission. This happens most of the time when people are in areas where bats are eating or are harvesting.
- Intermediate Hosts (the "Amplifier"): Bats are the primary source of the virus, and pigs are the "amplifier host." The virus spreads quickly in crowded pig pens, where it becomes more virulent before spreading to farmers or slaughterhouse workers.
- Environmental Persistence: The virus can live for days in contaminated liquids (like date palm sap) or on surfaces that are cool, which makes it more likely that one will come into contact with cool surfaces, increasing the likelihood that the most common way for the virus to spread from person to person is through blood, urine, or saliva from an infected person. This happens most often among family caregivers and healthcare workers.
- Super-Spreader Potential: In previous outbreaks, specific individuals (typically exhibiting severe respiratory symptoms) have been identified as "super-spreaders ", transmitting the virus to numerous individuals, resulting in substantial viral shedding in respiratory droplets.
What are the symptoms of Nipah Virus?
- Pain in the head
- Pain in the muscles
- Tiredness
- As the disease gets worse, severe Nipah virus symptoms like confusion, seizures, trouble breathing, and coma can show up in just a few days. Recognising the first signs of the Nipah virus early can make a big difference.
- Fever
- A very high fever
- Bad headache
- Changed mental state
- Breathing problem, very high fever, and manifestations in the brain
- In many reported cases of Nipah virus infection in India, neurological symptoms appear quickly after the onset of fever. Being infected can cause things to get worse quickly. Nipah infection occurs at the n-th fever onset.
Finding out if you have the Nipah virus
- Early Stage (Acute Phase): During the first 4 to 14 days of symptoms, the primary test is Real-Time RT-PCR. It detects viral RNA (specifically the primaryN gene) in body fluids before the immune system begins to fight back.
- Late Stage & Recovery: ELISA (Enzyme-Linked Immunosorbent Assay) is used to detect antibodies, such as IgG. RT-PCR finds the virus itself, while ELISA checks for such an immune response. This is very important for people who have been sick for a week or more.
- The "Gold Standard" for virus isolation is to grow the virus in a lab culture (Vero cells). Because it is so dangerous, this can only be done in Biosafety Level 4 (BSL-4) labs that are very secure.
- Post-Mortem Confirmation: When a patient dies before a diagnosis is made, immunohistochemistry is used to find viral antigens in tissue samples, like those from the lungs or brain
- The "Flu Mask": Nipah is often "detected late" because its early symptoms (fever, cough, headache) are similar to those of common seasonal illnesses, and doctors don't think of it right away.
- Sample Variety: To make sure the virus isn't missed, a diagnosis often requires more than one sample, such as throat swabs, blood, urine, and cerebrospinal fluid (CSF). This is because the virus could be in the lungs but not yet in the blood.
- Infrastructure Gaps: RT-PCR requires specialised equipment and trained personnel to operate in rural areas where specialised equipment is needed; it can take personnel time to transport samples to a central lab, such as the National Institute of Virology (NIV) in Alappuzha or Pune. This can delay life-saving isolation.
- Differentiating Strains: In Kerala, more advanced tests, like Next-Generation Sequencing, are being used to determine whether an outbreak is the "Bangladesh strain" (which spreads more widely) or the "Malaysia strain."
Treatment for the Nipah Virus?
- Help with breathing
- Management of the nervous system
- Water and Electrolytes
- Monoclonal Antibodies (m102.4): These antibodies, made in a lab, have shown promise in preventing the virus. A small number of people in India and Australia have used it.
- Remdesivir: This antiviral is used for COVID-19 and is effective in animal studies when administered shortly after exposure.
- Ribavirin was used in the first outbreak in Malaysia in 1999, but experts are still not sure how well it works.
- New Candidates (Update for 2026): Recent studies on oral medications such as VV116 (initially developed for COVID-19) have demonstrated the ability to reduce brain and lung inflammation in laboratory environments.
How to Prevent Nipah Virus?
- Don't eat fruits that bats have already eaten.
- Clean fruits well
- Stay away from people who are sick.
- Wear protective gear when working in healthcare settings
- Strong surveillance systems in India have enabled early detection of the Nipah virus. The most vigorous defence, bro, is early detection in Kerala; the most essential strategy is to stop Nipah.
Nipah Virus Outbreaks in India 2026
- Kerala (many outbreaks since 2018): Kozhikode, Malappuram, and most recently Palakkad have had the most cases in this area. Because Kerala has many people and many fruit bats, there is a high risk of "spillover."
- West Bengal (2001, 2007, and 2026): * Siliguri (2001): The first recorded Indian outbreak, with 75% of cases being healthcare workers or family members, shows how dangerous it is to get sick in a hospital.
- Barasat/Kolkata (January 2026): A recent outbreak with five confirmed cases, mostly among healthcare workers, has led to alerts across the country and screenings at international airports.
Ways to Manage
- The "Route Map" system: In Kerala, officials make and publish maps showing where an infected person has been. This makes people more likely to report themselves if they were at the same place, which is like the "early screening" approach you support for cancer care.
- 21-Day Strict Quarantine: India requires that any "primary contacts" (people who had direct contact with the infected) be quarantined for 21 days. This is because the incubation period can be.
- Quarantined containment: When a case is identified, a "containment zone" is established around the patient's home. Movement is limited, and health workers go from door to door to check for people with fevers.
- Alerts for news in real time: Mobile alerts and "Health Beware Cards" are now used at borders to keep an eye on travellers from areas that have been affected, like West Bengal or Kerala, and to monitor for illness.
The Nipah virus is still a public health issue.
Final Thoughts
If you experience any of the symptoms mentioned above, please contact Renova Hospitals for further evaluation and appropriate medical care.
Disclaimer
Category
- Joint Replacement
- Joint Replacement































































