Vitamin D supports cancer prevention by regulating cell growth, promoting apoptosis (programmed cell death), reducing chronic inflammation, and strengthening immune surveillance. Research shows that individuals with vitamin D levels above 40 ng/mL have a 67% lower risk of cancer compared to those with levels below 20 ng/mL (
PLOS ONE, 2018).
While vitamin D and reduced cancer mortality show promising correlations in research, it is not a standalone cure. Maintaining optimal vitamin D levels (30-50 ng/mL) may contribute to lower cancer risk when combined with screening, a healthy lifestyle, and medical care.
Key Takeaways:
- Vitamin D supports cancer prevention through cell cycle control, apoptosis, DNA repair, and immune modulation, but is NOT a cure or standalone therapy.
- Boosts immunity by enhancing macrophages, T-cell regulation, and suppressing inflammatory cytokines (IL-6, TNF-alpha) that fuel tumour growth.
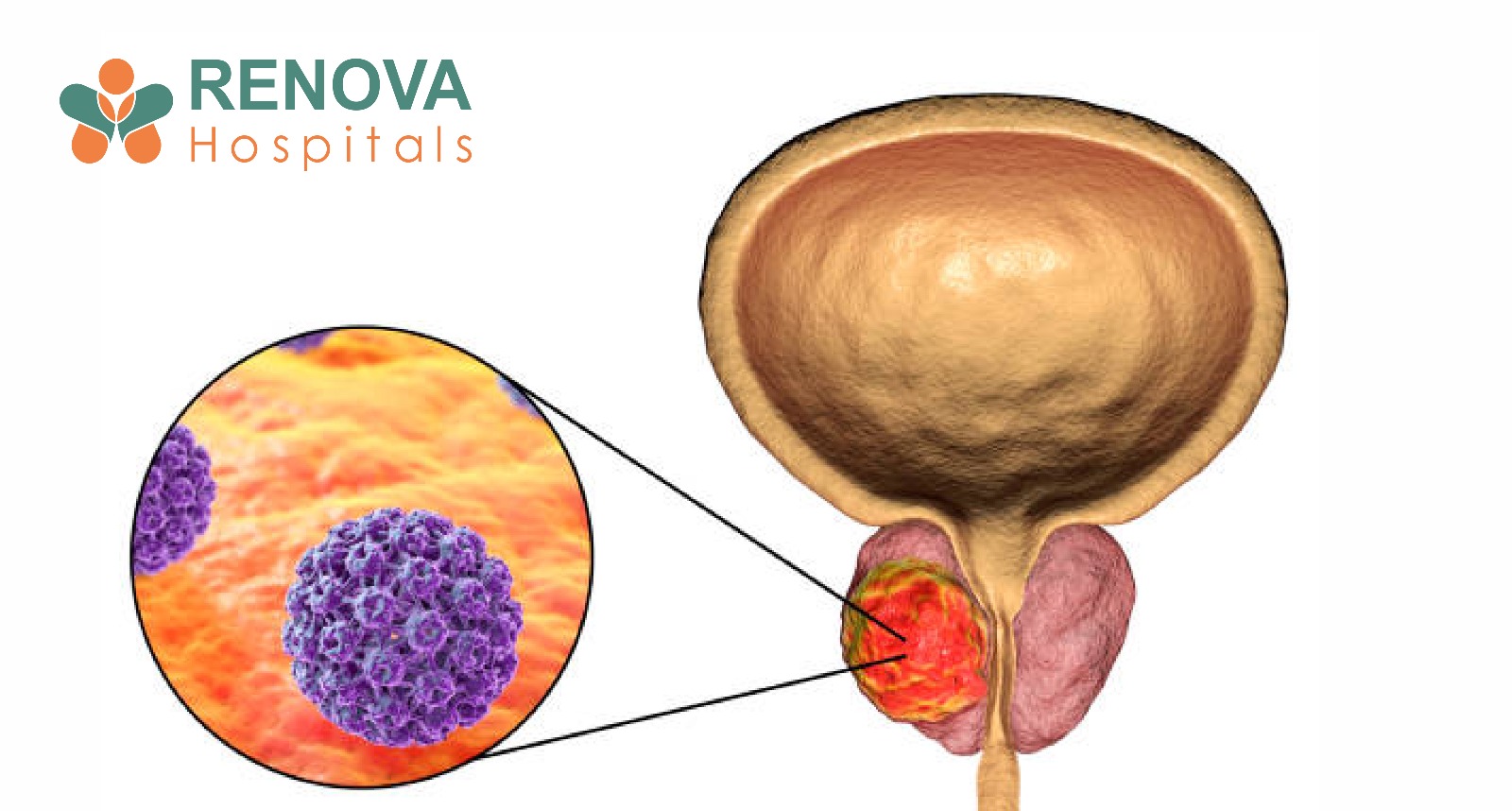
- Deficiency linked to higher colorectal, breast, and prostate cancer risk. Target levels: 30-50 ng/mL (sufficient); below 20 ng/mL (deficient).
- Best supplements: Vitamin D3 (cholecalciferol), liquid/softgel forms, with K2, third-party tested. Typical dose: 1,000-2,000 IU daily.
- Deficiency common in India (indoor living, pollution, skin pigmentation). Get tested if: limited sun, fatigue, cancer history, autoimmune disease, or obesity.
- May reduce cancer risk, but NOT guaranteed, requires screening, lifestyle changes, and medical care. Too much causes hypercalcemia and kidney stones.
Does Vitamin D Prevent Cancer?
Vitamin D may reduce cancer risk, but it does not guarantee prevention. Research shows that vitamin D and cancer prevention are linked through multiple biological pathways, including DNA repair, cell cycle control, and immune modulation. However, randomised controlled trials show mixed results. The relationship between vitamin D deficiency and cancer risk is stronger in observational studies than in intervention trials.
How Vitamin D Boosts the Immune System
How vitamin D boosts the immune system involves two critical defence mechanisms:
Innate Immunity (First-Line Defence)
Vitamin D strengthens your body's immediate response to threats by enhancing macrophage activation, stimulating antimicrobial peptide production, and improving pathogen recognition. Research shows vitamin D increases production of cathelicidin (an antimicrobial peptide) by over 300% (
Journal of Immunology, 2004). This rapid response system helps eliminate abnormal cells before they become cancerous.
Adaptive Immunity (Long-Term Protection)
Vitamin D regulates T-cell differentiation, suppresses excessive inflammatory Th17 responses, and promotes regulatory T cells (Tregs). This creates a balanced immune response to cancer, aggressive enough to detect threats but controlled enough to prevent harmful chronic inflammation.
The immune response to cancer depends heavily on this balance. Vitamin D helps your immune system distinguish between normal cells and cancerous ones while preventing autoimmune damage.
Why Vitamin D Is Being Studied in Cancer Research
Vitamin D acts as a steroid hormone in the body. After activation, it binds to the Vitamin D Receptor (VDR), which is expressed in more than 30 tissues, including colon, breast, prostate, lung, pancreas, and in critical immune cells (T cells, macrophages, dendritic cells). The VDR regulates approximately 3% of the human genome, over 2,700 genes (
Genome Research, 2010).
Scientific reviews published in peer-reviewed journals such as MDPI (Cancers, 2024) and The Journal of Steroid Biochemistry and Molecular Biology demonstrate that vitamin D regulates hundreds of genes involved in cell cycle control, DNA repair, immune modulation, inflammatory pathways, and tumour microenvironment regulation.
Because cancer develops when these protective systems fail, vitamin D and cancer prevention have become central to oncologic research.
How Vitamin D Regulates Abnormal Cell Growth
Cancer begins when cells divide uncontrollably due to genetic mutations. Vitamin D influences four critical anti-cancer mechanisms:
1. Cell Cycle Arrest
Vitamin D slows excessive cell division by regulating proteins such as cyclins and cyclin-dependent kinases. This prevents uncontrolled replication of damaged cells that could become cancerous.
2. Promotion of Apoptosis
Apoptosis is your body's natural "self-destruct" program for damaged cells. Vitamin D enhances pro-apoptotic signalling and suppresses survival pathways in abnormal cells, thereby ensuring that damaged cells are eliminated before they proliferate.
3. Support of Cellular Differentiation
Cancer cells often lose their specialised function and behave chaotically. Vitamin D promotes differentiation, encouraging cells to maintain their normal, specialised roles rather than becoming malignant.
4. DNA Repair Assistance
DNA damage accumulates over time due to oxidative stress and environmental exposure. Vitamin D influences pathways that repair damaged DNA before mutations become cancerous.
Can Vitamin D Reduce Tumour Growth and Spread?
Laboratory and animal studies suggest vitamin D may influence tumour progression through three key mechanisms:
Anti-Angiogenesis (Blocking Blood Supply)
Tumours require new blood vessels to grow beyond microscopic size. Vitamin D may suppress vascular endothelial growth factor (VEGF), potentially limiting tumour blood supply and starving cancer cells of nutrients. Studies show vitamin D can reduce VEGF expression by up to 50% in breast cancer cells (
Cancer Research, 2006).
Reduced Invasion and Metastasis
Vitamin D has been shown in experimental models to reduce epithelial-mesenchymal transition (EMT), a key process that allows cancer cells to break away from tumours and spread to other organs.
Modulation of Tumour Microenvironment
Vitamin D may reduce inflammatory cytokines within the tumour environment, making it less favourable for cancer progression. This contributes to the relationship between vitamin D and cancer survival rates.
Important caveat: Most of these findings are strongest in preclinical studies. Large-scale human trials show mixed outcomes, highlighting the complexity of vitamin D and cancer prevention in real-world populations.
Is Chronic Inflammation Linked to Cancer?
Yes. Chronic low-grade inflammation is a recognised driver of cancer development, contributing to DNA damage, tumour initiation, angiogenesis, and metastasis.
Vitamin D helps modulate inflammatory cytokines such as IL-6 and TNF-alpha, potentially lowering your body's long-term inflammatory burden. Studies show vitamin D supplementation can reduce IL-6 levels by up to 36% and TNF-alpha by up to 32% (
Nutrition & Metabolism, 2014).
A comprehensive review in
Nature Reviews Cancer (2007) highlighted this anti-inflammatory effect as a key reason researchers study vitamin D and reduced cancer mortality.
The immune response to cancer is significantly influenced by inflammatory signalling. By keeping inflammation in check, vitamin D helps create an environment less conducive to cancer development.
Vitamin D Deficiency and Cancer Risk
Observational studies consistently show that vitamin D deficiency and cancer risk are associated. A meta-analysis of 17 studies involving over 12,000 participants found that individuals with the highest vitamin D levels had a 50% lower risk of colorectal cancer compared to those with the lowest levels (
The BMJ, 2014).
Low serum vitamin D levels also correlate with increased risks of breast cancer and prostate cancer. Research published in
JAMA Oncology (2019) supports these associations.
Some research also suggests improved vitamin D and cancer survival rates. A study of 4,443 cancer patients found that those with sufficient vitamin D levels (>30 ng/mL) had a 19% lower overall mortality risk compared to deficient patients (
JAMA Network Open, 2019). Patients with sufficient vitamin D levels may experience better outcomes during treatment.
However, randomised controlled trials (RCTs) show mixed results. The landmark VITAL study involving 25,871 participants over 5.3 years found that 2,000 IU/day vitamin D3 supplementation did not significantly reduce total cancer incidence (HR 0.96).
However, there was a 25% reduction in cancer deaths among participants (
New England Journal of Medicine, 2019). This highlights an important scientific principle: association does not equal causation.
Vitamin D Deficiency Cancer Symptoms: What to Watch For
While
vitamin D deficiency cancer symptoms are not directly diagnostic of cancer, chronic vitamin D deficiency may present alongside increased cancer risk. Common deficiency signs include:
- Chronic fatigue and weakness
- Bone pain and muscle aches
- Frequent infections (immune dysfunction)
- Depression or mood changes
- Slow wound healing
If you experience these symptoms alongside unexplained weight loss, persistent pain, or other concerning changes, consult a physician for a comprehensive evaluation. These symptoms are nonspecific but warrant attention when considering overall cancer prevention.
What Are Optimal Vitamin D Levels?
Most clinical guidelines consider 30-50 ng/mL (75-125 nmol/L) as sufficient for cancer prevention and immune support. Levels below 20 ng/mL are considered deficient.
Supplementation should be individualised based on blood test results, age, body mass index, kidney and liver health, and genetic variations (VDR polymorphisms).
Is Vitamin D Deficiency Common in India?
Yes. Despite abundant sunlight, vitamin D deficiency is highly prevalent in India. Studies show that 70-90% of Indians are vitamin D deficient, with levels below 20 ng/mL (
Indian Journal of Medical Research, 2018). This is due to indoor lifestyles, limited direct sun exposure, air pollution, and skin pigmentation reducing UVB absorption. Urban populations show even higher deficiency rates of up to 94%.
Routine screening may be beneficial, especially for high-risk individuals concerned about vitamin D deficiency and cancer risk.
Best Vitamin D Supplements for Immunity
When choosing the best vitamin D supplements for immunity, consider:
- Vitamin D3 (cholecalciferol) over D2—D3 is more effective at raising blood levels
- Liquid or softgel forms for better absorption
- Products with added vitamin K2 to support calcium metabolism
- Third-party tested brands for quality assurance
- Typical dosing: 1,000-2,000 IU daily for maintenance (consult physician for higher doses)
Always consult a healthcare provider before starting supplementation to determine the appropriate dose for your specific needs.
Are There Risks of Taking Too Much Vitamin D?
Excessive vitamin D supplementation can cause hypercalcemia (high blood calcium), kidney stones, cardiac rhythm disturbances, and vascular calcification.
High-dose self-medication is not recommended. Always consult a physician before long-term supplementation, especially if you're taking vitamin D specifically for cancer prevention.
Who Should Get Their Vitamin D Levels Tested?
Consider testing if you have limited sun exposure, chronic fatigue, are undergoing cancer treatment, have autoimmune disease, have obesity, have a family history of cancer, or are elderly.
Testing is simple and helps guide safe supplementation while monitoring vitamin D deficiency and cancer risk factors.
What Does Current Scientific Evidence Conclude?
Current research on vitamin D and cancer prevention supports that vitamin D regulates gene expression involved in tumour biology, supports immune surveillance, modulates inflammation, and may improve cancer outcomes in certain contexts.
However, it is not a standalone therapy. It does not replace chemotherapy, surgery, radiation, or immunotherapy. Vitamin D should be integrated into comprehensive care plans.
Ongoing clinical trials continue to evaluate optimal dosing, target populations, and the potential therapeutic role of vitamin D in cancer treatment and prevention.
Vitamin D and Cancer Prevention
Vitamin D plays a scientifically credible role in supporting immune health and influencing biological pathways linked to cancer development. Maintaining adequate vitamin D levels supports immune regulation, reduces chronic inflammation, and helps control abnormal cell growth.
However, cancer prevention requires a multi-layered approach that includes regular screening, tobacco cessation, healthy weight maintenance, physical activity, balanced nutrition, and evidence-based medical care.
If you are concerned about cancer prevention, immune health, or vitamin D deficiency, consult a qualified physician for personalised testing and guidance.